Impacted Canines
Overview
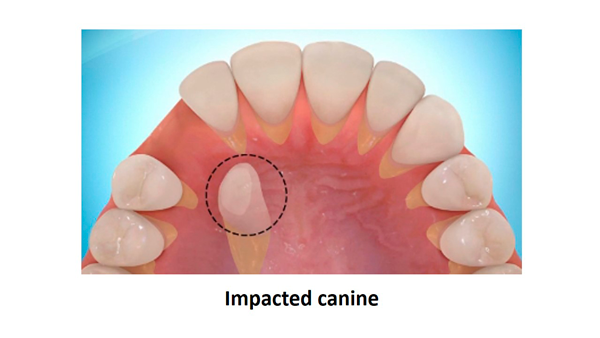
In some cases, teeth do not erupt properly through the jawbone and gum tissue, into the mouth. Maxillary canines (upper eye teeth) are the most commonly impacted, after wisdom teeth. Impacted teeth may cause problems including bone loss, root resorption, or formation of cysts or tumours. Your Orthodontist and Oral & Maxillofacial Surgeon can work together with a combination of braces and minor surgical procedures, including tooth exposure & bonding of an orthodontic bracket, to bring the tooth properly in alignment with the other teeth. Surgical procedure can be completed while awake, or with a variety of anaesthesia options.
What are Impacted Canines and Impacted Teeth?
An impacted tooth is one that does not properly erupt into the mouth. The most commonly impacted teeth are wisdom teeth, followed by the maxillary canines (upper eye teeth). The canines are important teeth as they frame your smile, and are also important for chewing. However, any tooth could potentially become impacted, for numerous reasons.
Impacted canines occur in 2% of the population, affecting twice as many females as males, and twice as many in the top jaw as the bottom jaw. This can sometimes occur on both the right and left. The majority of impacted canines are located on the roof of the mouth.
There are many reasons that teeth may become impacted. In some cases there may not be enough room in the jaw for them to fit. In other cases, they cannot follow the normal track along adjacent teeth to erupt into proper position. Other theories suggest a genetic component may be a contributing factor in impacted teeth, and may be associated with other dental abnormalities.
Diagnosis of Impacted Canines and Teeth
How do we find out if a canine or other tooth is impacted? And how do we find out where it is?
The first method is easy – observation and palpation. Adult teeth should erupt at certain ages; if they’re missing, then there may be a problem. In addition, the angulations and positions of adjacent teeth may give a clue as to the position of the missing tooth. Careful examination of the area, along with feeling along the gum tissue, may give a hint as to the missing tooth’s position.
X-rays are typically the next step in gathering information. In most cases nowadays, a 3-D Cone Beam CT scan is taken, which provides detailed 3-dimensional information about the impacted tooth’s position in relation to the jaw and adjacent teeth, the effect on adjacent teeth and structures, and for planning purposes.
Problems from Impacted Canines and Teeth
 Impacted canines and teeth that are left in place may go throughout the patient’s lifetime with no untoward effects. However, close monitoring and at regular dental care intervals is recommended. On the other hand, these impacted teeth may have several untoward effects and consequences.
Impacted canines and teeth that are left in place may go throughout the patient’s lifetime with no untoward effects. However, close monitoring and at regular dental care intervals is recommended. On the other hand, these impacted teeth may have several untoward effects and consequences.
The simplest problem is that a tooth will be missing from the smile. Although sometimes a baby tooth will be retained in that position, it will never have the proper shape and size that an adult tooth will have. In the worst-case scenario, there will be a gap that is visible beside the rest of the teeth.
Impacted teeth may also cause damage to adjacent teeth, known as resorption. In resorption, the impacted tooth “eats away” at a portion of the healthy tooth. Many times this is unrestorable, and in rare cases may actually cause loss of the tooth.
If resorption does not occur, adjacent teeth may be pushed out of their normal positions from pressure of the impacted tooth, causing mal-alignment.
Pathology can sometimes develop around an impacted tooth. Pathology usually represents an abnormal growth of tissue around the tooth, typically in the form of a cyst or tumour. While there are many different variations and types of cysts and tumours, treatment at a minimum would require removal of the lesion and possibly removal of the impacted tooth. Worst case scenarios would result in loss of adjacent teeth, and possibly need for further surgical treatment to ensure that the lesion does not recur.
Treatment of Impacted Canines and Teeth, including Exposure and Orthodontic Bonding
Treatment for impacted canines can vary.
In some cases, removing the baby canine can create enough space for the adult tooth to drop into position. This would usually be done around 10-13 years of age. However, this does not guarantee correction or elimination of the problem. The tooth should be monitored and, if not corrected or improved after a year, additional treatment should be undertaken.
Surgical treatments exist to help bring an impacted canine or tooth into proper position. Selection of the type of procedure depends on which tooth is impacted, the degree of impaction, and the position of the tooth within the jaw bone.
- Gingivectomy (Open Exposure) can be used, where overlying gum tissue is simply removed to allow the tooth to erupt naturally, or to allow the orthodontist to bond an attachment to it directly.
- Apically positioned flaps are used to expose the tooth through the gum tissue, but also to create a healthy band of gum tissue around the tooth.
- Exposure and bonding involves uncovering the impacted tooth and bonding an orthodontic attachment to it, then replacing the gum tissue over the tooth. The attachment is connected to a gold chain that is used to apply gentle traction to coax the tooth into position.
Extractions are sometimes considered with some impacted teeth. However, it is seldom a good idea to extract an impacted canine. Not only are the canines important aesthetically in the smile, but they are also important in a functional bite. The rare situation where canine extraction might be considered include: ankylosis, where the tooth is “stuck” and will not come into position; it is undergoing resorption which indicates an inflammatory reaction is compromising the tooth; there are pathologic changes like cysts or tumours, as mentioned above; the impaction is severe, and is jeopardizing adjacent teeth; or if the patient does not want to pursue orthodontic treatment.
Steps in Treatment
In cases where the canine will not erupt spontaneously, the orthodontist and oral surgeon work together to get these unerupted canines to erupt. Each case must be evaluated on an individual basis but treatment will usually involve a combined effort between the orthodontist and the oral surgeon. The most common scenario will call for the orthodontist to place braces on the teeth (at least the upper arch). A space will be opened to provide room for the impacted tooth to be moved into its proper position in the dental arch. If the baby canine has not fallen out already, it is usually left in place until the space for the adult canine is ready. Once the space is ready, the orthodontist will refer the patient to the oral surgeon to have the impacted canine exposed and bracketed.
In a simple surgical procedure performed in the surgeon’s office, the gum on top of the impacted tooth will be lifted up to expose the hidden tooth underneath. If there is a baby tooth present, it will be removed at the same time. Once the tooth is exposed, the oral surgeon will bond an orthodontic bracket to the exposed tooth. The bracket will have a miniature gold chain attached to it. The oral surgeon will guide the chain back to the orthodontic arch wire where it will be temporarily attached. Sometimes the surgeon will leave the exposed impacted tooth completely uncovered by suturing the gum up high above the tooth or making a window in the gum covering the tooth. Most of the time, the gum tissue will be returned to its original location and sutured back with only the chain remaining visible as it exits in the future position of the tooth.
Shortly after surgery (1-2 weeks) the patient will return to the orthodontist. A rubber band will be attached to the chain to put a light eruptive pulling force on the impacted tooth. This will begin the process of moving the tooth into its proper place in the dental arch. This is a carefully controlled, slow process that may take up to a full year to complete. Remember, the goal is to erupt the impacted tooth and not to extract it! Once the tooth is moved into the arch in its final position, the gum around it will be evaluated to make sure it is sufficiently strong and healthy to last for a lifetime of chewing and tooth brushing. In some circumstances, especially those where the tooth had to be moved a long distance, there may be some minor “gum surgery” required to add bulk to the gum tissue over the relocated tooth so it remains healthy during normal function. Your dentist or orthodontist will explain this situation to you if it applies to your specific situation.
What can I expect after surgery?
You can expect a limited amount of bleeding from the surgical sites after surgery. Although there will be some discomfort after surgery at the surgical sites, most patients find Paracetamol and/or Ibuprofen to be adequate to manage any pain they may have. All necessary prescriptions will be given to you in advance. Within 2-3 days after surgery there is usually little need for any medication at all. There may be some swelling from holding the lip up to visualize the surgical site; it can be minimized by applying ice packs to the lip for the afternoon after surgery. Bruising is not a common finding at all after these cases. A soft, bland diet is recommended at first, but you may resume your normal diet as soon as you feel comfortable chewing. It is advised that you avoid sharp food items like crackers and chips, as they will irritate the surgical site if they jab the wound during initial healing. Mr. Erasmus will see you 7-10 days after surgery to evaluate the healing process and make sure you are maintaining good oral hygiene. You should plan to see your orthodontist within 1-2 weeks to activate the eruption process by applying the proper rubber band to the chain on your tooth.
Mr. Erasmus is happy to work with you, your Orthodontist, and your Dentist for your dental health. You may be referred for evaluation and to discuss the options for the tooth. Please contact us if you have any questions about this procedure.