Corrective Jaw / Orthognathic Surgery
What Is Orthognathic Surgery?
Orthognathic surgery is also known as “Surgical Orthodontics” and the treatment involves the skills of both an Orthodontist and an Oral and Maxillofacial Surgeon. An Orthodontist can move the teeth while the surgeon is able to surgically reposition the jaw(s). The aim of orthognathic surgery is to surgically reposition the jaw(s) to establish a normal relationship between the upper and lower jaws, which will facilitate the orthodontic positioning of the teeth into a normal bite. The benefits include an improved ability to swallow, chew, speak and breathe. In many cases an important benefit is an enhanced facial balance and appearance.
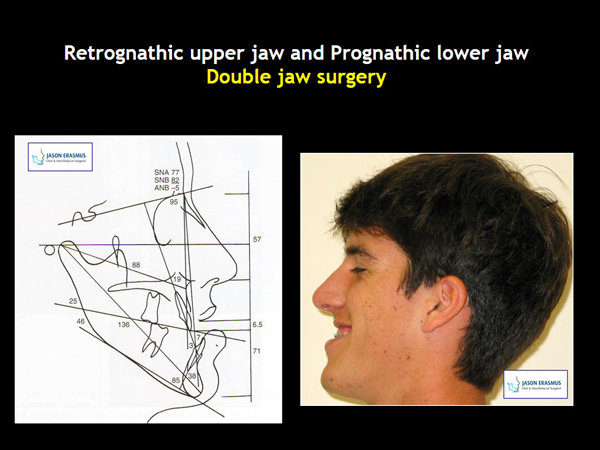
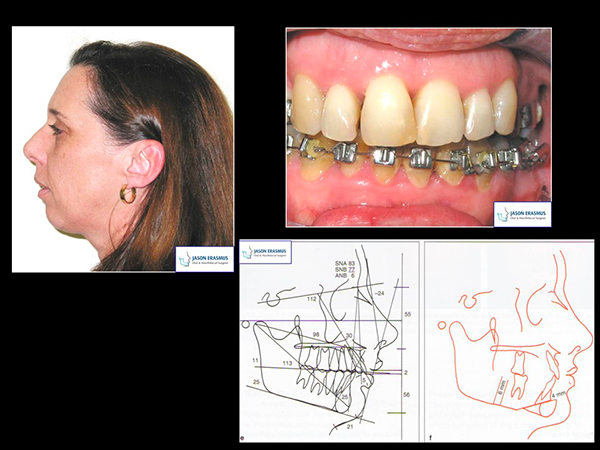
Gallery
- All patients have given their permission for the use of their photos on this website for educational purposes
- All these cases were operated by Mr Jason Erasmus
- Photos are copyright protected
Who Needs Orthognathic Surgery?
Many bite problems can be treated with braces (orthodontics) alone however improper bite problems that also involve abnormal jaw positions will benefit by a combination of tooth alignment (orthodontics) and surgical correction of the jaw position (orthognathic surgery). Orthodontic treatment only for an inappropriate bite of individuals with abnormal jaw positions often has disadvantages such as: complex and prolonged treatment time, poor long term stability, and compromised aesthetic outcomes. In severe cases it is impossible to treat people without a combination of orthodontics and surgery.
Jaw growth is a slow and gradual process and one or both jaws may grow too much, too little or asymmetrically. Injury to the jaws and birth defects can also effect the alignment of the jaws. The abnormality may lead to poor tooth alignment with difficulty in chewing food properly, abnormal speech, swallowing and or an abnormal breathing pattern. The tongue may be forced to move awkwardly during speech and swallowing in an attempt to compensate for the abnormal tooth and jaw relationship. There may be a speech defect (i.e. lisping, nasality) and excessive mouth breathing. Chronic mouth breathing bypasses the physiological benefits of the nose during the normal breathing pattern. The nose cools hot air, heats cold air, moistens dry air and captures dust particles before the air reaches the lungs. An abnormal bite may also threaten the long term health of the gums (periodontitis) and teeth (excessive wearing). The joints between the lower jaw and the skull (temporomandibular joints) can also be adversely affected by a malrelationship between the jaws (i.e. pain, clicking, locking). Jaws of different sizes often adversely affect the facial balance and appearance.
The following are some conditions that may indicate a need for orthognathic surgery:
- Difficulty in chewing or biting food
- Difficulty in swallowing
- Speech problem
- Chronic joint pain
- Excessive wearing of teeth
- Open bite (the front teeth don’t meet)
- Facial injury
- Cleft lip and palate
- Receding chin
- Pronounced and or asymmetric lower jaw
- Inability to make lips meet without effort
- Chronic mouth breathing with dry lips and mouth with bleeding gums
- Sleep apnea (snoring, difficulty breathing affecting normal peaceful sleep)
In order to determine if you are a candidate for orthognathic surgery, discuss your symptoms with your dentist, orthodontist, or oral and maxillofacial surgeon.
Particulars of Evaluation, Treatment Planning, and Treatment
Pre-treatment evaluation and treatment planning
Unequal jaw positions, improper bites, and symptoms that require orthognathic surgery will demand a team approach that usually include the general dentist, an orthodontist, and a maxillofacial and oral surgeon. In order to diagnose your need for orthognathic surgery and to formulate a detailed treatment plan the team members need to work closely together. The orthodontist is responsible for moving (aligning) the teeth so they will fit together following surgical repositioning of the jaw(s). The surgeon is responsible for repositioning the jaw(s) to establish a normal relationship between the jaws, a functional and stable bite, and facial harmony. Your general dentist will be responsible for maintaining your oral health before, during, and after treatment.
After clinical examination and subsequent detailed analysis of your records (dental casts, x-rays and photographs), a diagnosis is made and a treatment plan is prepared. Once a definitive treatment approach has been established the patient will be informed about the orthodontic and surgical treatment envisaged. It is advisable that the patient is accompanied by parents/husband or wife (as applicable) to this case presentation by either the orthodontist or surgeon.
A Typical Treatment Profile

Stage1: Placement of orthodontic braces
Should the treatment plan require extraction of some teeth (including wisdom teeth), this is done, and usually two to three weeks later the orthodontic bracketss are fitted to the teeth.
Stage 2: Pre-operative orthodontics (9-18 months)
During this phase the teeth will be aligned in their optimal position as planned, in each jaw. No attempt will be made to correct the bite, which in some cases may actually become worse (i.e. the under bite or overjet may increase). This treatment phase will usually take on average between 9 and 18 months depending on the severity of the problem and patient cooperation. When the orthodontist is satisfied that the preparation is complete, the patient is referred back to the surgeon.
Stage 3: Surgery
The surgeon will now surgically reposition the jaw(s) into their most favourable relationship to establish a good occlusion (bite) and balanced facial proportions. After a short healing period of two to three weeks the patient returns to the orthodontist for the final correction of the bite (see notes below – “The Surgical Phase”).
Stage 4: Post-operative orthodontics (3-6 months)
The purpose of orthodontic treatment after the surgery is to refine the bite and usually involves minor tooth movement to finalize the bite. Once the orthodontist is satisfied with the result the brackets are removed. Patients often become very impatient to complete the treatment at this stage. It is however worthwhile to persist to achieve the best possible result. Keep in mind that the treatment is performed to last for the rest of your life and will probably be one of your most valuable assets.
Stage 5: Retention (12-24 months)
When the orthodontic treatment has been completed the teeth that have been moved through the bone need to be stabilized in their new positions for a period of time. The orthodontist manufactures and fits a retention appliance, which must be worn by the patient as instructed by the orthodontist.
The Surgical Phase
Pre-surgical records: When the team determines that your teeth are in the correct planned position, surgery will be scheduled. Your surgeon will use new x-rays and models of your teeth and jaws to simulate the surgical movements of the jaw(s) and to predict anticipated soft tissue changes. The surgeon may prefer to make a plastic wafer to serve as a guide for accurate surgery.
Preparation for surgery: Orthognathic surgery is performed in a hospital under general anesthetic and in most cases you will be admitted into the hospital on the day of surgery. Prior to surgery you will have a physical examination to ensure you are in good overall health. Your anaesthetist will discuss the anaesthetic procedure to be used and answer any questions you may have. You may receive medication to reduce normal pre-surgical anxiety.
Surgery: Whilst there are a variety of surgical procedures that may be used those most frequently selected include: surgery to the lower jaw, the upper jaw and chin surgery.
Read in more detail about these three surgical procedures.
Post surgical period: Following completion of your surgical procedure, you will be transferred to the recovery room. There, your progress will be monitored closely by the nurses on duty. You will remain in the recovery room for about one hour until you are sufficiently awake to be transferred to your room. Occasionally, it may be necessary to send you to the High Care Ward where you will receive more intensive nursing during the first few hours following your surgery.
Post-operative pain: In most cases the procedure is surprisingly less painful than expected however a certain amount of pain must be expected and the necessary painkillers will be provided. The discomfort is usually worse than the pain and may last for a few days to a fortnight.
Swelling: You can anticipate that swelling will occur and the degree of swelling is quite variable amongst individuals. More swelling usually occurs with lower jaw surgery than with upper jaw surgery. Swelling will increase for approximately 48-72 hours following surgery. At the completion of the surgery a soft pressure bandage will be placed over your jaw to assist in controlling the swelling. While your head will be slightly elevated during the period of hospitalization, ice packs will be placed on your jaws to further reduce the swelling.
Minor bleeding following surgery: It is common to experience some degree of bleeding following surgery, and minor nose bleeds may be expected for a period of 1-2 weeks following upper jaw surgery. This may be more pronounced when leaning forward. However, if bleeding continues for longer than 15-20 minutes contact your surgeon immediately.
Nausea and vomiting: You may experience some nausea and vomiting. This is sometimes the result of the anaesthetic or an irritation of old blood in your stomach. Therefore, if vomiting does occur, remain calm, and turn your head to the side so that any fluid produced clears your mouth freely. The nurses who care for you are used to dealing with patients who have had this type of operation and are properly trained to cope with this effect.
Physiotherapy: Many surgeons will recommend post-operative physiotherapy treatment in order to:
- Decrease the degree of swelling and bruising
- Help reduce pain
- Accelerate healing
- Minimize scar tissue formation
- Restore normal jaw function
Numbness: A numbness of the lower lip and chin may be expected following lower jaw and chin surgery while the upper lip, cheeks, palate, and gums may feel numb following surgery to the upper jaw. This is due to interference with the nerves supplying sensation to these areas and is usually temporary. Feeling can be expected to return to these areas within a few weeks following surgery however may even take several months to return. Unfortunately, in a very small percentage of cases, this may be permanent.
Nasal stuffiness: The cause of nasal stuffiness may be either from the tubes placed during surgery or from the surgical procedure in the upper jaw surgery. When this occurs, it can be managed with a combination of nasal sprays and cleaning the nostrils.
Blowing of the nose: Do not blow your nose or sneeze with your mouth closed for at least 1 week following upper jaw surgery. This can cause air to be forced into your cheeks and lower eyelids with immediate severe swelling. A nasal spray will be provided to help decongest the nasal passages.
Medication: An intravenous infusion will be attached to your arm during surgery to provide required medication and nutrients until you are able to take sufficient liquids by mouth. During the period of hospitalization, you will usually be given antibiotics, pain medication, an anti-inflammatory, mouth wash, and medicated cream for your lips and for upper jaw surgery – a nasal spray. Most of the medication will be continued on discharge from hospital. It is important to utilize your medication as prescribed.
Elastics: Elastics are generally used to stabilize the jaws and to guide the teeth into the new bite. They are usually placed immediately after the operation, and should not be removed until the first post-operative appointment. At your first post-operative visit the surgeon will instruct you how to apply and use the elastics. The elastics should be used as directed until your next appointment with your orthodontist.
Cleaning your teeth: It may be difficult to clean your teeth during the first few days following surgery. It is however advantageous to clean your teeth after each meal and you fortunately, you will have sufficient time to do it! A small soft tooth brush can be utilized for this purpose and in addition a mouth rinse should be used. Soak the bristles in the mouth wash and brush slowly, in order to get maximum benefit from the antiseptic effect of the mouth wash.
Clear liquids: An adult requires approximately 2-3 liters of fluid every 24 hours as a normal fluid intake. Although this may seem like a large quantity, it can be achieved with constant sipping. It will be important that you drink a sufficient volume of fluid to allow the discontinuance of the drip on the following day. Once you have fully recovered from the after effects of the anaesthetic, you will be encouraged to drink clear liquids. This will often be easier directly from a cup or glass due to the loss of sensation in the lips. However a large catheter tipped syringe will be available to assist you if you find this method easier.
Splints: In selected cases, the use of a splint is necessary. This is a plastic template made after the dental casts have been positioned into the planned new bite. The splint is constructed of clear plastic (acrylic) and the teeth are wired into the splint to establish and maintain the correct jaw position. It is not visible to the casual observer and will remain in place until bone healing has been completed.
Wiring the teeth together: With the use of rigid fixation (small plates and screws) which will hold the jaw segments together, it is seldom necessary to wire the jaws together. However in some selected cases it may be advantageous depending on the technique used. The necessity for this will be discussed with you prior to the operation.
Day of discharge and healing phase: Most patients are ready for discharge within two days after surgery. A period of rest for up to one week is recommended and after that you are encouraged to resume your normal activities as soon as possible. Although you may resume with light physical exercises after 10 days, contact sport should be avoided for at least six weeks following surgery. It is very important for the treatment team to be sure that all the oral and facial tissues adjust to their new relationship that bone healing is normal and that final soft tissue settling takes place. You would therefore see the surgeon or orthodontist for regular evaluation visits. It is important to keep in mind that although 90% of the post-operative swelling disappears within the first 10-14 days, the initial healing phases will take approximately 6 weeks. Completion of the healing and firming up of the muscles can only be expected after 6-10 months.
Diet: It is vitally important that chewing forces applied to the operated jaws are kept to a minimum during the first 3-4 weeks following surgery. Under no circumstances are you to chew solid foods. It is suggested that prior to your jaw surgery you acquire a blender and a food strainer. The usual post-operative program is: one or two days of liquids followed by a week of pureed foods and then three weeks of soft foods. Food and nutrition plays a vital role in our daily lives, especially where healing needs to take place. A soft diet can still be balanced providing all the necessary nutrients. It is important that all the components required for your rehabilitation should be available to your body. You may select foods that you can manage. In order to ensure that you have a balanced diet, try and include something from each food group at each meal. A weight loss of approximately 3Kg may be anticipated during the post operative period. This is a reflection in most cases of loss of appetite, rather than the soft diet. By one week following surgery, your appetite should be sufficiently improved to maintain and possibly increase your weight.
It is very important to realize that the bulk consumed with liquid diet is not sufficient to satisfy an appetite. Hunger or appetite is relieved by distention of the stomach, chewing, and the volume consumed, and a liquid or soft diet may not satisfy these demands. Thus more frequent intake is required and it is strongly recommended that your diet is taken as a breakfast, morning tea, lunch, afternoon tea, supper and before retire. This will keep the hunger pangs at bay!
Read more about Known Risks and Complications of Orthognathic Surgery.
General
If you are not sure about any part of your treatment, please ask your Orthodontist or Mr Erasmus who will only be too pleased to help. Feel part of the team and enjoy the progress during treatment.
The aim of your treatment is to move your teeth and jaw(s) into a new position that is more balanced, functional, and healthy. This should enable you, not only to bite and chew better than before, but your speech as well as swallowing pattern and in many instances breathing pattern may be enhanced. In addition your facial balance will be restored. The results of your Orthognathic surgery can have a dramatic and positive effect on many aspects of your life.
SO… make the most of it!